Welcome to 𝘑𝘢𝘯𝘴𝘴𝘦𝘯 𝘞𝘪𝘵𝘩 𝘔𝘦® Ireland
Information and support for patients, relatives and carers

Disease areas
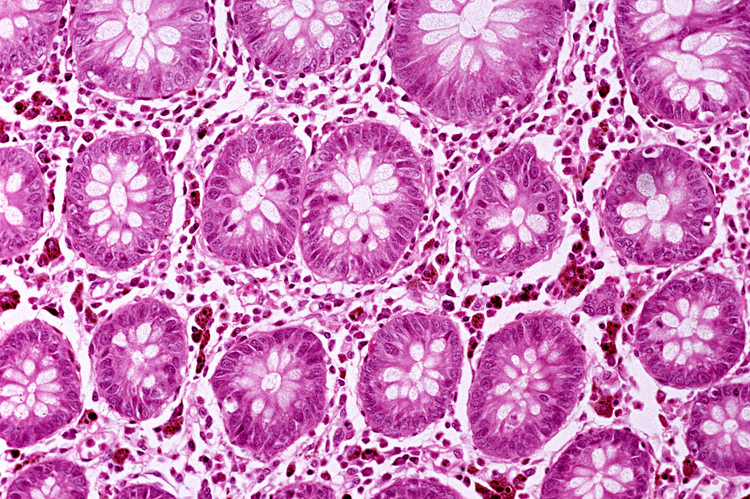
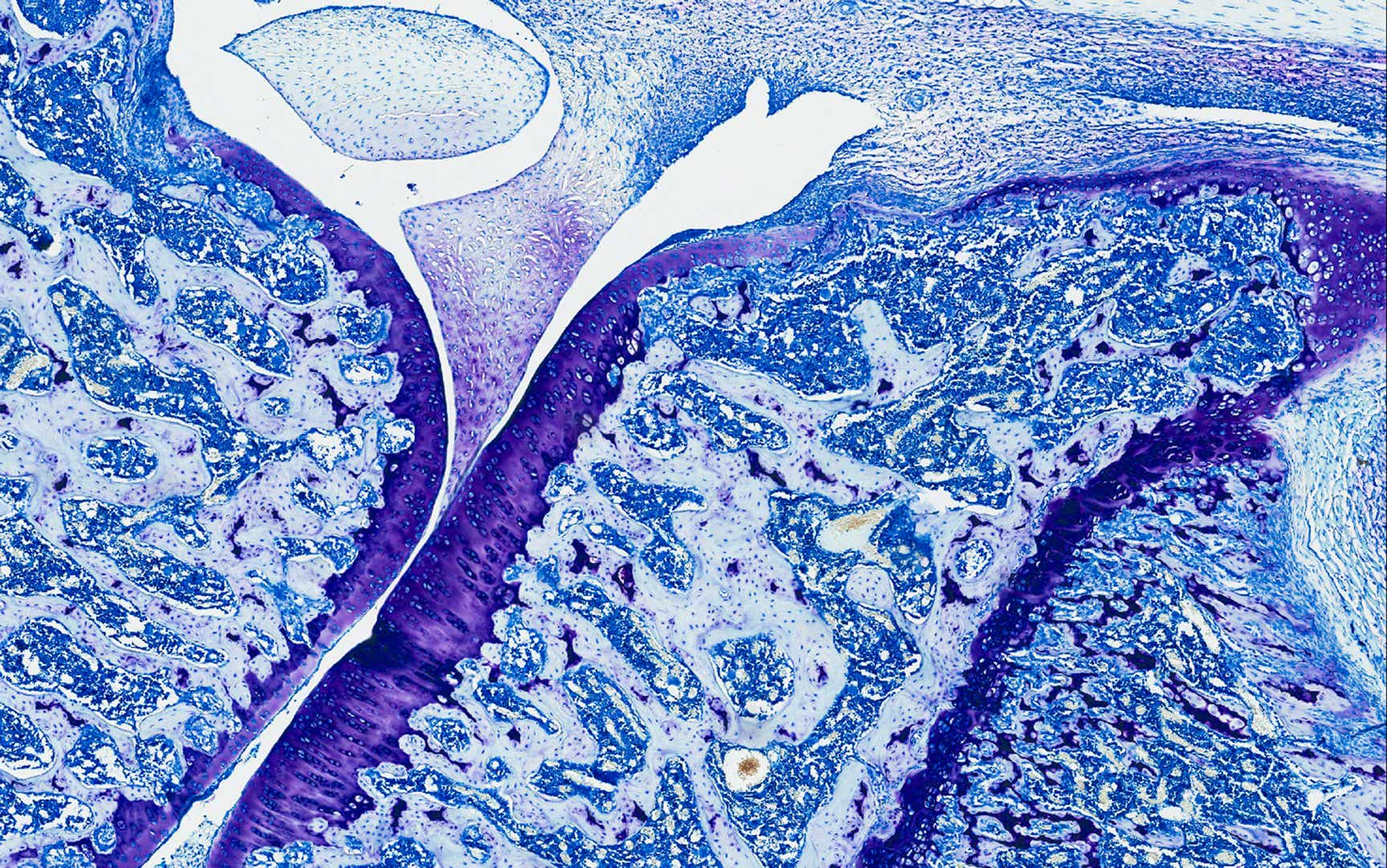
Inflammatory Bowel Disease
Mental Health
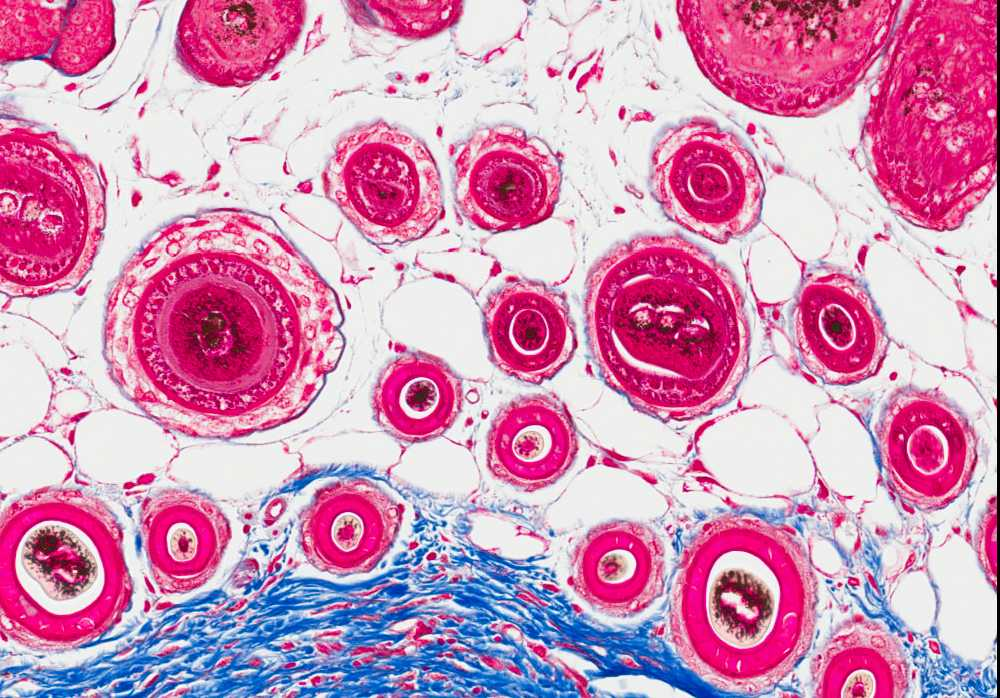
Prostate Cancer
Psoriasis
Psoriatic Arthritis
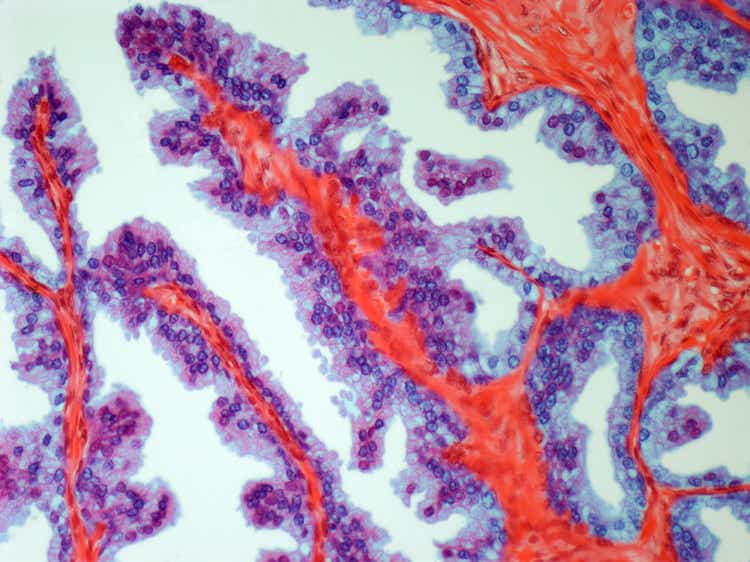
Pulmonary Arterial Hypertension
Our initiatives

Talking Depression aims to support people living with depression and their loved ones, by providing helpful information and resources.

Information and support to help you be more than your psoriasis or psoriatic arthritis.

For anyone living with a rare, chronic condition, such as Pulmonary Hypertension, having access to practical support and resources can be extremely valuable.

MyIBDJourney offers guidance on how to plan and manage the range of symptoms you may encounter as an individual living with Inflammatory Bowel Disease, allowing you to live your life to the fullest.
Information placed on this digital platform is not intended as a substitute for consultation with your healthcare professional. Please consult your healthcare professional for further information.
.png?width=750&height=502&format=png&quality=50)